UCSF REACH will redefine how clinicians understand, diagnose, and treat patients with chronic low back pain
San Francisco (Oct. 9, 2019) — This week, the UCSF Dept. of Orthopaedic Surgery received NIH funding totaling more than $30 million to establish the UCSF Core Center for Patient-centric, Mechanistic Phenotyping in Chronic Low Back Pain, or UCSF REACH. The new center will conduct both translational and clinical research to clarify biopsychosocial mechanisms of back pain – the interconnection between biology, biomechanics, psychology, and socio-environmental factors – which will be catalytic for new therapeutic, diagnostic and prevention strategies.
From left to right: Jeffrey Lotz, PhD; Conor O’Neill, MD; Aaron Fields, PhD; Jeannie Bailey, PhD; and Dezba Coughlin, PhD.
UCSF REACH will be led by Jeffrey Lotz, PhD, the David S. Bradford M.D. Endowed Chair in Orthopaedic Surgery, and Vice Chair of Research within the Department, and Conor O’Neill, MD, Director of the Department’s Non-Operative Spine Program in the UCSF Spine Center.
Dr. Lotz will serve as the director of the administrative core, and Dr. O’Neill will serve as director of the clinical trials core. Other key members of the center’s leadership team from Orthopaedics will include: Aaron Fields, PhD, who will be leading center’s pathophysiology core, Jeannie Bailey, PhD, who will be leading the center’s biomechanics core, and Dezba Coughlin, PhD, who will be leading the center’s operations.
REACH integrates investigators across UCSF and the UC Health System, including the Department of Epidemiology & Biostatistics, the Department of Family and Community Medicine, the Department of Radiology & Biomedical Imaging, the Department of Physical Therapy & Rehabilitation Science, the San Francisco VA Medical Center, the Bakar Computational Health Sciences Institute, and the Department of Neurological Surgery.
Need for REACH
According to the Global Burden of Disease Study 2010, low back pain is one of the most common forms of chronic pain among adults worldwide.
As recently as 2015, the National Health Interview Survey indicated that 20 percent of adults in the U.S. reported frequent back pain and 28 percent experienced low back pain that lasted one or more days during the previous three months.
“There is no accepted clinical standard for diagnosing chronic low back pain, and consequently, clinicians are often unable to identify the root cause,” Lotz said. “Back pain is the leading cause of disability and healthcare expenditures worldwide, as well as the leading non-cancer reason for opioid prescription in the U.S.”
In an effort to reverse the nation’s opioid crisis, the National Institutes of Health recently awarded $945 million to institutions across 41 states for grants, contracts and cooperative agreements to support its Helping to End Addiction Long-term Initiative, known as HEAL.
As part of HEAL, the NIH formed the Back Pain Consortium (BACPAC) Research Program, a translational, patient-centered effort to address the need for effective, non-addictive, and personalized therapies for chronic low back pain.
The national collaboration is composed of mechanistic research centers and technology development sites that will combine translational research and Phase 2 clinical trials to deliver an integrated model of chronic lower back pain. UCSF was awarded three of the program’s 13 grants.
“Our goal over the next five years is to develop an integrated model of low back pain supported by a suite of validated diagnostic tests,” Lotz added. “In doing so, clinicians will be more precise in treating the problem, which should naturally lead to lowering patients’ dependency on opioids to manage their pain.”
The REACH program combines an interdisciplinary research team with expertise in basic and clinical sciences:
- behavior and brain function
- pathophysiology and advanced imaging
- clinical trials
- physical function and biomechanics
- machine learning and artificial intelligence
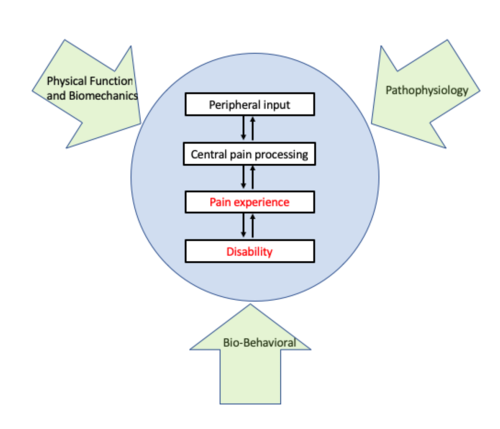
Three UCSF REACH research cores align with domains in the biopsychosocial model of chronic low back pain. Infographic courtesy of Conor O’Neill, MD
Developing technology to provide best treatment options
In addition to REACH, there will be two UCSF Technology sites that will work with the research team to develop tools to help clinicians identify specific low back pain and help physicians determine who are best for certain therapies.
“By leveraging state-of-the-art imaging and computing tools, we will develop new algorithms that will enable clinicians to precisely diagnose and treat their patients with the best options suited for them,” said Aaron Fields, PhD, who was awarded $1.1 million to lead one of UCSF’s Technology sites in a joint collaboration with Roland Krug, PhD (UCSF Dept. of Radiology and Biomedical Imaging).
Interdisciplinary care, evidence-based approaches for managing a broad spectrum of spinal disorders
"Our community of physicians who care for patients with disorders of the spine includes surgeons, physiatrists, anesthesiologists, neurologists, physical therapists radiologists, and medical and alternative health specialists,” said Sigurd Berven, MD, chief of service for the UCSF Spine Center. The Spine Center is one of the largest centers for management of spinal disorders in the U.S., and a leading center for the development of evidence-based approaches to manage disorders of the spine based upon rigorous assessment of outcomes and clinical research.
“This grant will provide an important opportunity for our community of physicians and therapists to work together to translate discoveries in diagnostics and therapeutic interventions to clinical care of patients," added Dr. Berven.
“These NIH-supported programs will establish precision medicine approaches to manage chronic lower back pain,” said Dr. Thomas P. Vail, Chair of the Department. “By supporting transdisciplinary collaborations among investigators and other BACPAC programs, REACH’s goal will be to integrate advanced technologies and validated instruments to classify patients for targeted therapies that optimize their chance of a good outcome.”
###
Media contact
For media inquiries and interview opportunities, please contact Kathleen Jay (kathleen.jay@ucsf.edu), Marketing Manager, UCSF Dept. of Orthopaedic Surgery