Spine Tethering
(Also known as Vertebral Body Tethering, VBT, Anterior Spinal Growth Tethering.)
Traditional treatments for scoliosis – bracing and spine fusion surgery – improve the condition but come at a cost. Bracing, while physically appearing benign, has psychological consequences that are real but difficult to qualify and quantify. Spinal fusion stops a scoliotic curve from getting worse by stopping motion between vertebrae, the bones that make up the spinal column. The part of the spine operated on no longer moves at all, which alters the function of the spine. The patient can not reach for things in the same way. Children may no longer be able to participate in their sport because of limited movement. The rest of the spine that is not fused has to do extra work, because it has to compensate for the loss of movement at the fused spine; as a result, the unfused spine wears out more quickly, which leads to degenerative arthritis.
As a result, UCSF's Dr. Mohammad Diab, along with select centers nationwide, conceived a new approach to scoliosis: fusionless surgical tethering of the spine. This treatment modulates spinal growth, guiding the spine to grow straight – something bracing can't do – while maintaining the motion that fusion eliminates. Back in 2007 when Dr. Diab began tethering (along with Dr. Betz of Philadelphia at the time), this was a novel procedure and as such had not been approved by the Federal Food and Drug Administration (FDA), which regulates medical devices. In 2019, FDA approved the procedure, easing insurance approval for patients.
There are three principal effects of tethering on the spine:
-
Curve progression is arrested, because the cord will not stretch and therefore will not allow the the convex side of the spine to grow.
-
Motion is preserved in all directions except the undesirable one, along the convexity where the scoliosis would increase.
-
Concave (on the side of the spine opposite the surgery) growth is not affected, which promises spontaneous and complete (if there is sufficient growth remaining) correction as the child grows.
The last effect is impossible in a brace, which can only stop progression and can not correct a curve. The last effect is impossible with spinal fusion and instrumentation, which corrects incompletely all at once and produces a fixed spine that can not move and can not change.
What is the system used to tether?
The system consists of screws connected by a cord. The screws are made of titanium and coated with hydroxyapatite, which is the mineral framework of bone. The coating is believed to help the screws interdigitate or lock to bone, making them more stable. The cord is made of polyethylene terephthalate (known commercially as polyester, the same material used in fabrication of marine sails and plastic water bottles), connects the screws. The cable resists stretching in the direction of the scoliosis, but allows for movement in every other direction, including opposite the scoliosis, forward and backward, and turning.
What patient will benefit from tethering?
Curve between 40°-70°
Below 40° fusion is not indicated, so observation or bracing are the correct treatments. Bracing is initiated at 30°, so by the time a curve reaches 40° there has been sufficient experience to show that bracing has failed. At that point, tethering may be considered as an alternative to fusion. Above 70°, the screw-cord construct may not be strong enough to hold the curve. In addition, the bigger the curve the more growth is necessary to correct it.
Growth remaining.
This is difficult to calculate precisely. General guidelines include before periods for a girl and absent Risser sign on X-rays. Exceptions may be made in certain cases, for example where maturity signs are not consistent, or for lumbar curves where the loss of motion is significant. Age as a cutoff is arbitrary, but as a rule too young (< 10 years) may result in over-correction, and too old (> 14 years) may not allow for growth modulation and spontaneous correction because of too little growth remaining. Hand X-rays are unreliable.
Preoperative evaluation.
X-rays are obtained to measure the curve (in degrees) standing and lying down, measures flexibility as the spine is unloaded by taking away the effect of gravity. Flexibility is further determined by asking your child to bend to the right and to the left, to see how much a curve will “open up”.
An MRI of the spine is obtained in children younger than 10 years, to evaluate the nerves of the spine, including the spinal cord, since nerve tissue does not appear on X-rays and may be abnormal in this age group with scoliosis. Depending on the child, sedation by and Anæsthesiologist may be necessary, because an MRI of the spine requires that the child stay still for up to an hour.
In addition to X-rays, Dr. Diab obtains a computed tomography with angiography test. This studies the arteries that travel to the spine, to make sure there is no artery that critically feeds the spinal cord with blood. If one is detected in the part of the spine that will be operated on, Dr. Diab will skip that level. This will enhance the safety of the procedure without compromising the result.
Your child will be evaluated by the Prepare Clinic, which is staffed by Nurse Practitioners and A Anæsthesiologists. This visit will focus on all of your child’s health, and will identify areas of concern that require further work up.
If you wish, we can connect you with other patients of Dr. Diab who have undergone the procedure. We believe that patients can learn a lot from – and support – each other. This also applies to parents, who worry and need to hear from other parents how to get through this. We have many happy and smart patients who are keen to help and are a great resource!
Procedure
Your child is admitted to hospital on the day of operation. The operation takes about six hours and is performed under general anæsthesia. You will receive periodic updates from the circulating nurse in the operating room.
Thoracic curves are tethered from the front (anterior). The front of the convex side of the spine is reached by making an incision on the side of the chest and going between the ribs. The lung on that side of the chest is deflated by the Anæsthesiologist to allow an unencumbered view of the spine, and reinflated at the end of the procedure so it returns to normal function. A screw is inserted into the body (front part) of each vertebra. The cord is inserted into each screw. The screws are compressed to reduce the magnitude of the curve. The screws are tightened finally to maintain the correction. A chest tube is placed to collect blood, so it does not fill up the chest and interfere with lung function. The chest tube is connected to a receptacle that collects and measures the blood that drains. The chest tube is removed on the second day after surgery (by then bleeding has stopped and clotted off). The chest tube is uncomfortable, and limits how deeply the child breathes. Removing the chest tube is stressful, but it doesn’t hurt much and is a relief because after that the child can breathe normally again.
Lumbar curves may be tethered from the front or the back. If front (anterior), the incision is on the flank, the chest is entered, the diaphragm is cut (then repaired at the end of the procedure) and the abdominal organs are moved away. Because the chest is entered, a tube is inserted as for thoracic curves.
A lumbar tethering from the back (posterior) is performed by through a straight midline incision directly over the spinous processes (the bumps one can feel) of the lower half of the back. The muscles of the back are spread (between muscles, which are not cut) to reach the vertebræ to place the tethering system. Because the chest is not involved, no chest tube is necessary.
A catheter is placed in the bladder before the start of the procedure, to drain urine. This is kept in place for the first 1-2 days, so that your child does not have to get up to pee when pain might not allow this, or use a bed pan, which can be embarassing. Screws are inserted with the assistance of an X-ray machine that is rolled into the operating room. A neural physiologist is present throughout the procedure to monitor function of the nerves and spinal cord, on a computer connected with electrodes placed on your child’s head and limbs. A brace is worn after lumbar tethers, because of the greater flexibility of the spine, to protect the mineral coating of the screws as it locks with the mineral of the vertebral bone.
Recovery
After the operation, your child is admitted to the intensive care unit for close monitoring. A parent can stay with the child at all times. Pain medications will be delivered IV until your child is eating, after which they will be tablets or liquid by mouth. Pain medications have side effects, including slowing breathing, dizziness, nausea, and constipation (which can be more uncomfortable than pain). The best way to manage these side effects is to take only the pain medication amount that is necessary to make the pain manageable. It is unrealistic and unsafe to have the goal of making the pain go away: that would require too high a dose, which would produce too many side effects. Another way to reduce the side effects is to move, in particular walking. On the first day after operation, your child will get out of bed with the assistance of a physiotherapist and walk, the frequency and the distance of which will increase every day. While in the hospital, your child is fitted for a custom spine brace if necessary, which is worn for three months after the operation to allow the implants to lodge securely in the vertebræ.
Your child will be discharged from the hospital 2-4 days after the operation. The length of stay is determined primarily by your child’s comfort with pain and your comfort to be at home. Before discharge, the incision will be checked and redressed, all tubes and catheters removed, and X-rays will be obtained to make sure implants are stable after mobilization. Your child will return home with pain medications, as well as a brace if necessary.
Your child will return for a follow-up visit one week after operation to check in with Dr. Diab, including evaluation of the surgical wound. After that visit, your child may shower. Dr. Diab will obtain X-rays of the spine at three months after the operation, when a brace if worn will be discontinued. Most children return to school 1 month after surgery, and to full and unrestricted activity after the 3 month visit. We do not restrict children with tethers from any activity, except to say that the same rules for safety and common sense apply as for nonsurgical patients. Your child will return for annual or more frequent check-ups (according to growth) throughout growth until maturity, to look for any change in the scoliosis.
The screws and cord can not be felt by your child. The tether will be removed or exchanged only if the scoliosis completely corrects, in order to avoid the spine curving in the opposite direction, or if the curve keeps getting worse despite the tethering, such as when the cord breaks. In either case, your child will not feel it and will not be at risk. Otherwise, the implants do not need to be removed. Your child won't notice them in any way and the spine will remain mobile.
Dr. Diab gets many patients who come from far away, including from out of state. For such patients, he asks that you come the weekend before surgery, so that there is time to have a full evaluation (including imaging studies and a visit to the Prepare Clinic). He also asks that you plan to stay through the first postoperative visit during the week after discharge. He always wants to see his patients for follow up care. However, if you live far away, we can arrange video visits, including getting local X-rays and uploading them MyChart so he may review them with you. Finally, Dr. Diab has friends and colleagues all over the country, and he can arrange local orthopaedic and spine care as you may need.
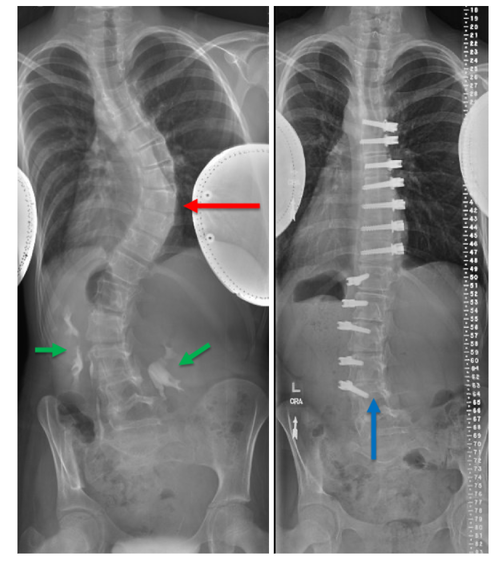
11 year old girl before surgery and 2 years after. The thoracic curve was tethered anterior, through the side of the chest to reach the front of the spine (red arrow). The lumbar (flank) curve was tethered posterior, through a midline incision (blue arrow). Contrast is being expelled by the kidneys (green arrows) after a computed tomography with angiogram test to study the blood flow to the spinal cord.