Primary Care Sports Medicine Fellowship Program
Welcome to the UCSF Primary Care Sports Medicine Fellowship
Our ACGME accredited program provides comprehensive training in Primary Care Sports Medicine. We focus on excellence in patient care, clinical research, teaching, and community advocacy and outreach with the goal of training the future leaders in sports medicine.
The program has a strong group of clinical faculty from various backgrounds, specialties, and training. We provide coverage to a wide variety of athletes including professional soccer, NCAA Division I through Cal, professional ballet and theatre, high school, adaptive sports, and mass participation events. Our fellow works as part of a multidisciplinary team which includes consulting physicians, athletic trainers, physical therapists, sports nutritionists, strength and conditioning specialists, orthotists & prosthetists, and psychologists throughout our core clinical training sites in the Bay Area. We also offer robust ultrasound experience, well-rounded educational didactics, support for scholarly activity, and multiple teaching opportunities
We currently accept one Family Medicine candidate each year. If you have any additional questions, please feel free to contact Will Dunbar at william.dunbar@ucsf.edu.
Application Process
Fellowship Positions: We offer 1 fellowship position each year (Family Medicine residency trained only).
Combined Salary and Housing Allowance (AY2025-26): $106,127
Duration: 1 year
Dates: July 1, 2026-June 30, 2027
Deadline for Applications: August 10, 2025
Apply through: ERAS/AAMC: https://students-residents.aamc.org/training-residency-fellowship/applying-fellowships-eras
Minimum Letters of Recommendation: 3
Please forward signed AMSSM code of ethics and first page of publications to program coordinator Will Dunbar at orthoeduteam@ucsf.edu.
In accordance with Federal and State law and University policy, the University of California does not discriminate on the basis of age, gender, race, ethnicity, national origin, religion, sexual orientation, gender identity, health, or disability. For detailed information, visit the Office for the Prevention of Harassment and Discrimination.
Read our Anti-Discrimination Policy. We are committed to upholding UCSF's PRIDE values and adhering to UCSF's Principles of Community.
Interviews
The Program Director and Application Selection Committee will review each application and select individuals who will be invited to interview. In accordance with the University of California Graduate Medical Education, we will be holding interviews virtually for the 2026-2027 application season. A "virtual social" and informational session will be held the evening before the interviews.
Interview Dates:
- Friday, October 3, 2025 - virtual AM (PT)
- Friday, October 10, 2025 - virtual AM (PT)
Program Curriculum
Our curriculum focuses on providing a broad spectrum of knowledge for diagnosis and treatment of exercise and sports related injuries, as well as illnesses in patients of all ages and abilities. This includes prevention, evaluation, management, and rehabilitation of injuries, as well as the effects of disease on exercise and the use of exercise in the treatment and prevention of medical problems. Our fellows become skilled in the uses and limitations of imaging and other procedures in diagnosing and treating these problems and are competent in properly using and/or prescribing physical therapy, massage, manipulations, therapeutic injections, imaging, musculoskeletal ultrasound, and sub-specialty consultation in the management of these problems. In a group practice with family physician and other primary care doctors, the fellow will also serve as a consultant for a wide range of musculoskeletal and exercise-related problems.
Sample Schedule:
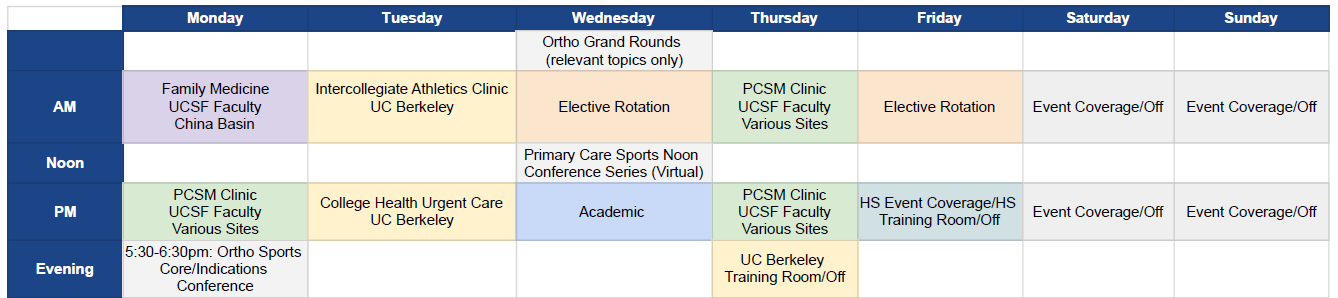
Longitudinal & Continuity Clinics
- 2-3 half-days per week devoted to providing Primary Care Sports Medicine (pediatric and adult)
- 2-3 half-days per week devoted to providing Division I Intercollegiate athlete care and college health center urgent care for both medical and MSK issues
- 1 half-day per week devoted to providing Family Medicine
- 1 half-day per week with high school athletes/training room
- 1 half-day per week of academic time
Elective Rotations/Clinics/Didactics (2 half-days 2 per week devoted to elective rotations)
- Orthopaedic Sports Medicine including surgical observation
- Orthopaedic Hand/Upper Extremity
- Orthopaedic Foot and Ankle
- Non-operative Orthopaedic Spine (Physiatry)
- Orthopaedic Pediatric Sports Medicine including pediatric fracture clinic, cast and splint application, pediatric/adolescent surgical cases
- Rheumatology
- Neurology
- Multidisciplinary Concussion Management: Neuropsychology, Optometry, and Neurology
- Sports Psychology/Psychiatry
- Sports Nutrition
- Sports Cardiology
- Skeletal Bone Health
- Orthotics and Prosthetics
- Physical Therapy
- Exercise Physiology & Biomechanics (UCSF Human Performance Center)
- Strength and Conditioning
- Physical Therapy
Ultrasound Curriculum
Our musculoskeletal ultrasound curriculum follows the AMSSM guidelines for sports medicine fellowships. Our fellow becomes proficient at diagnostic ultrasound of the 6 major body regions (shoulder, elbow, hand/wrist, hip, knee, ankle/foot) as well as common ultrasound-guided injections and procedures. A breadth of procedural opportunities is available, which includes joint injections, tendon sheath injections, nerve-blocks, hydro dissections, platelet rich plasma, and Tenex. Advanced topics in ultrasound (brachial plexus, abdominal wall, peripheral nerves, etc) is also available if the fellow is interested.
The curriculum is structured around dedicated monthly, hands-on didactics (more is available if the fellow is interested) and regular scanning practice with faculty. Cadaver labs have also been available for the fellow to practice more advanced injections and scans.
Our fellow will be issued a handheld Butterfly iQ ultrasound to use during the year and will have access to an ultrasound unit at nearly every clinical site.
By the end of fellowship, the fellow should have the knowledge to teach ultrasound at a national conference if the opportunity arises.
Scholarly Activity
UCSF offers a wealth of academic resources to support scholarly inquiry. Our fellow completes a research project and/or book chapter/case report/review article intended for presentation and/or publication. One half-day per week is dedicated towards scholarly activity. Further research support is provided by our primary care sports medicine research faculty mentors and by attending monthly research meetings. In prior years, fellows have presented at national conferences and been published in peer-reviewed journals.
Event Coverage Experience
Our fellowship program offers a variety of coverage experiences at multiple levels, including high school, NCAA Division 1 intercollegiate athletics, professional sports, ballet/dance, and mass participation sporting events. Our fellow learns the skills needed to serve as a team physician for a wide variety of sporting disciplines at varying levels. The fellow will work closely with orthopedic surgeon specialists, athletic trainers, physical therapists, coaches, nutritionists, psychologists, podiatrists, chiropractors, and other health care professionals in providing comprehensive care for athletes.
The fellow will gain valuable learning opportunities through coverage of:
- UC Berkeley (Cal) NCAA Division 1 school providing care to elite collegiate athletes in 27 varsity sports including football and rugby.
- High school athletics (Lowell High School)
- Oakland Roots USL Professional Soccer
- Oakland Soul Women’s USL Soccer Team
- Marathons, triathlon and cycling events
- Community dance/ballet
- Adaptive sports event coverage
- Community events: mass participation PPEs for local high schools with cardiac screening
We are proud that our fellowship program has been asked to assist with sports medicine care of elite athletes at the international stage. Our prior fellows have been involved with:
- Women’s National Basketball Association (WNBA) “Wubble” in Bradenton, FL (July 2020) – Fellow, Dr. Ginger Cupit
- International Surf Association’s World Para Surfing Championships in Pismo Beach, CA (December 2021) – Fellow, Dr. Pete DeJong
- International Surf Association’s World Surfing Championships in Huntington Beach, CA (September 2022) – Fellow, Dr. Ryan Wei
- International Surf Association's World Para Surfing Championships in Huntington Beach, CA (October 2023) - Fellow, Dr. Frances Tao
- International Surf Association's World Para Surfing Championships in Huntington Beach, CA (November 2024 - Fellow, Dr. Haley Oosterhouse
Didactics & Conferences
Core Didactics
Primary Care Sports Medicine Noon Conference Series: this weekly series reviews core topics in primary care sports medicine (see list below) from UCSF faculty and invited speakers throughout the nation. Conference attendees include primary care sports medicine attendings from around the greater Northern California area, other primary care sports medicine fellowship programs, physical therapists, athletic trainers, and registered dieticians. The fellow will be responsible for also presenting at this conference throughout the year with journal clubs and case conferences.
Orthopaedic Sports Core/Indications: this weekly meeting is collaborative between Primary Care Sports Medicine, Orthopaedic Sports Surgery and MSK Radiology. Challenging musculoskeletal cases are presented at the Ortho Sports Indications conference, coordinated with imaging findings. Didactic lectures are also presented during these meetings, followed by a journal article review and discussion.
UCSF Department of Orthopaedic Surgery Grand Rounds: these occur weekly and include varying topics in Orthopaedic Surgery with invited speakers from UCSF and other institutions. There are also lectures focused on faculty development. The fellow is expected to attend lectures on relevant topic areas.
Research Meeting: each month the fellow can attend the sports research meeting where faculty, fellows and research assistants present their research projects to the group. This is a great way for the fellow receive feedback/support for their academic projects.
Ultrasound Didactics: we have a robust ultrasound curriculum which includes monthly dedicated hands-on instruction (more is available if the fellow is interested) and regular scanning practice with faculty. Fellows have also attended cadaver labs to practice more complicated scans and injections. More in-depth information can be found by reviewing our ultrasound curriculum.
PCSM Fellow Didactic Lecture + Workshop Topics
|
Injuries + problems of the
Physical exam of the
Fracture care
|
Additional musculoskeletal topics
|
Medicine topics
|
Team doctor topics
|
Conferences
The fellow gains valuable experience attending various conferences throughout the year both regionally and nationally. A set amount of CME funding is provided to the fellow each year to help with some costs. These conferences can include:
- American Medical Society for Sports Medicine (AMSSM) Fellow’s Research & Leadership Conference
- AMSSM Annual Meeting
- UCSF Inman Abbott Society Conference
- American College of Sports Medicine (ACSM) Annual Meeting (optional)
- Pediatric Research in Sports Medicine (PRiSM) conference (optional)
The fellow also serves as a lecturer for continuing education courses hosted by UCSF:
- UCSF Primary Care Sports Medicine Conference (December)
- UCSF Pediatric Sports Medicine and Orthopedic Conference (March)
UCSF Primary Care Sports Medicine Faculty
 |
 |
 |
 |
|
| Nicolas Hatamiya DO | Cindy J. Chang MD | Anthony Luke MD MPH | Carlin Senter MD | Bill Berrigan MD RMSK |
 |
 |
 |
 |
|
| Tyler Padgett DO | Lindsay Huston MD | Amy White Hockenbrock MD | Matthew Lynch MD | Celina de Borja MD |
 |
 |
 |
 |
|
| Rhonda Watkins MD MPH | Faustine Ramirez MD, RMSK | Zach Bailowitz MD, RMSK |
Core Primary Care Sports Medicine Faculty at UCSF
Nicolas Hatamiya, D.O. (Family Medicine/Sports Medicine)
|
|
Dr. Nicolas Hatamiya is the current Program Director for the Primary Care Sports Medicine Fellowship. He is a Clinical Assistant Professor with the UCSF Department of Orthopaedic Surgery. He earned his medical degree from Western University of Health Sciences and completed his residency in Family Medicine at Stanford Health Care - O’Connor Hospital, where he served chief resident. He completed a fellowship in Primary Care Sports Medicine at UCLA, where he served as a team physician for the UCLA Bruins and assisted with the Los Angeles Lakers and Los Angeles Dodgers. He is an active member of the American Medical Society for Sports Medicine and held numerous leadership positions as a medical student, resident and fellow. In 2019, he was awarded the AMSSM Resident Scholarship and in 2020 received the AMSSM Local Humanitarian Service Project Grant. His research interests include sports medicine applications of digital health technologies, musculoskeletal ultrasound, and improving sports medicine training in medical education. Hatamiya currently is a Team Physician for the Oakland Roots Professional Soccer Team. |
Carlin Senter, M.D. (Internal Medicine/Sports Medicine)
|
|
Dr. Carlin Senter earned her medical degree at UCLA, completed residency in internal medicine at the University of Washington and a fellowship in primary care sports medicine at UCLA. Dr. Senter belongs to the American College of Physicians, American Medical Society for Sports Medicine, American College of Sports Medicine and Society of General Internal Medicine. She has received numerous awards for teaching and community service. Dr. Senter’s goal is to help every patient be an athlete. She has particular interests in exercise counseling, exercise prescription and sports concussion, for which she co-directs the UCSF Sports Concussion Program. Dr. Senter's research focuses on enhancing musculoskeletal education for primary care clinicians. She designs programs to increase knowledge of the musculoskeletal system and improve diagnostic skills among medical students, residents and practicing clinicians. She co---chairs two annual UCSF Continuing Medical Education sports medicine courses, chairs the Clinical Skills Committee for the American College of Physicians and is the program planning co-chair for the American Medical Society for Sports Medicine 2021 Annual Meeting. An avid athlete, Dr. Senter rowed for Radcliffe crew throughout college. She has served as team physician for several high school teams throughout the Bay Area and is currently team physician for the University of San Francisco. |
Anthony Luke, M.D., MPH (Family Medicine/Sports Medicine
|
|
Dr. Anthony Luke trained in family medicine at the University of Toronto followed by a fellowship in sports medicine at the Children’s Hospital of Boston and Master’s of Public Health at Harvard. His research interests include injury prevention in youth sports, running medicine and digital health. Dr. Luke is medical director of several large Bay Area sports events, such as San Francisco Marathon and Escape from Alcatraz, and works with runners including an injury prevention program he created called RunSafe™. He is also director of the Human Performance Center and Primary Care Sports Medicine program, and holds the position of Benioff Distinguished Professor in Sports Medicine. He helps direct UCSF’s Sports Medicine Center for Young Athletes program, which provides sports medicine services to more than 30 public and private high schools in the Bay Area. |
William A. Berrigan, M.D., RMSK (Physical Medicine and Rehabilitation/Sports Medicine)
|
|
Dr. Bill Berrigan earned his medical degree from St. George’s University SOM and trained in Physical Medicine and Rehabilitation (PM&R) at Medstar Georgetown-NRH. He completed a two-year fellowship in Primary Care Sports Medicine at Emory where he served as chief fellow, focused on research and academic leadership. At Emory, he was the head team physician of the Fan Controlled Football League and assistant team physician for the College Park Skyhawks, the G league affiliate of the Atlanta Hawks, while also assisting with the Falcons, Hawks, and Dream. Dr. Berrigan specializes in diagnostic ultrasound, advanced ultrasound-guided procedures, and orthobiologics. His research interests include ultrasound shear wave elastography and the evidence-based use of orthobiologic treatments. |
Faustine Ramirez, M.D., RMSK (Pediatrics/Sports Medicine)
|
|
Dr. Faustine Ramirez earned her medical degree and completed residency in pediatrics at UCSF. She completed a fellowship in primary care sports medicine at Stanford University, where she served as team physician for the varsity football, women's soccer, and men's and women's gymnastics teams, and provided comprehensive care for varsity student-athletes across all sports. Her clinical and research interests include bone health and bone stress injuries, overuse injuries, youth sports specialization, diagnostic musculoskeletal ultrasound, and care of the female athlete. |
Core Family & Community Medicine (FCM) Faculty at UCSF
Tyler Padgett, D.O.
|
|
Dr. Tyler Padgett is an Associate Physician Diplomate with the UCSF Department of Family & Community Medicine. He earned his osteopathic degree from Kansas City University of Medicine and Biosciences College of Osteopathic Medicine. He still practices and teaches osteopathic manipulation technique (OMT). He went on to complete his residency in Family Medicine at David Grant Medical Center, Travis Air Force Base, in Fairfield California. He was an ESPN Academic All American Kicker for his college football team, the Central Methodist Eagles. He served six years in the United States Air Force where he earned a Meritorious Service Medal. His personal hobbies include golf and bicycling. is an Associate Physician Diplomate with the UCSF Department of Family & Community Medicine. He earned his osteopathic degree from Kansas City University of Medicine and Biosciences College of Osteopathic Medicine. He still practices and teaches osteopathic manipulation technique (OMT). He went on to complete his residency in Family Medicine at David Grant Medical Center, Travis Air Force Base, in Fairfield California. He was an ESPN Academic All American Kicker for his college football team, the Central Methodist Eagles. He served six years in the United States Air Force where he earned a Meritorious Service Medal. His personal hobbies include golf and bicycling. |
Primary Care Sports Medicine Faculty at UC Berkeley
Lindsay Huston, M.D. (Family Medicine/Sports Medicine)
|
|
Dr. Lindsay Huston received her medical degree from the University of California, Davis, and completed her family medicine residency through Kaiser Permanente Los Angeles. She finished her training at the San Jose-‐O'Connor sports medicine fellowship under Dr. Michael Henehan. Following her fellowship, she became head team physician at Yale University. After four years there, she returned to her native Bay Area to join the sports medicine staff at UC Berkeley, and was named Cal head team physician in 2016. Dr. Huston has served as head team physician for both Yale University and the University of California, Berkeley, two of the largest NCAA Division I athletic programs in the country. Her interest in collegiate sports medicine began when she was a varsity softball player as an undergraduate at Stanford University. In addition to caring for all of Cal’s 850 athletes, Dr. Huston sits on the board of the Pac-‐12 Student-‐Athlete Health and Well Being Initiative. |
Amy White Hockenbrock, M.D. (Family Medicine/Sports Medicine)
|
|
Dr. Amy White Hockenbrock was an undergraduate at U.C. Berkeley where she studied Molecular and Cell Biology and led Cal’s women’s soccer team to multiple playoff berths from 1996 through 2000. She received her M.D. from Chicago Medical School and then returned to San Jose for residency and primary care sports medicine fellowship at O’Connor Hospital. Following fellowship, Dr. White Hockenbrock was an attending physician at Family Medicine Associates of San Jose before joining West Coast Sports Institute. From 2018-‐2019 she worked for Planned Parenthood as Interim Transgender Program Director for the Mar Monte region. In January of 2020, Dr. White Hockenbrock recently rejoined the Cal community as an Associate Team Physician, bringing her experience and skills in sports medicine, LGBTQ care and women's care to U.C. Berkeley. |
Matthew Lynch, M.D. (Internal Medicine/Sports Medicine)
|
|
Dr. Matthew Lynch is a Board Certified Primary Care Sports Medicine and Internal Medicine physician focusing on care of the student athlete at the University of California, Berkeley. Dr. Lynch earned his bachelor’s degree from Yale University, his medical degree at Eastern Virginia Medical School and completed residency in Internal Medicine and fellowship in Primary Care Sports Medicine at the University of Cincinnati. He has cared for a range of athletes of all ages and abilities, from weekend runners to professional soccer players. Prior to moving to UC Berkeley, Dr. Lynch was the team physician for Miami University of Ohio, Yale University, University of California, Davis and FC Cincinnati professional soccer team. |
Additional Primary Care Sports Medicine Faculty
Cindy J. Chang, M.D. (Family Medicine/Sports Medicine)
|
|
Dr. Cindy Chang is Professor Emeritus at UCSF and the founder of the UCSF Primary Care Sports Medicine Fellowship Program. She is currently the Chief Medical Officer of the NWSL. She trained in family medicine at UCLA under Dr. Jim Puffer, followed by a fellowship in sports medicine at The Ohio State University (OSU) with Dr. John Lombardo. Dr. Chang remained on OSU faculty as assistant residency director and assistant team physician before becoming head team physician at the University of California, Berkeley for all 27 sports, including football, in 1995. At Cal, she was the site director for the UC---Davis/UC--- Berkeley Primary Care Sports Medicine fellowship for 13 years. She has served as Team USA’s chief medical officer at the 2008 Beijing Paralympics and 2012 London Olympics. She is Past President of the American Medical Society for Sports Medicine (AMSSM) and is on the Board of Trustees for the American College of Sports Medicine (ACSM), and is a Fellow of both AMSSM and ACSM. Dr. Chang has served on the Sports Medicine Advisory Committee (SMAC) for the National Federation of State High School Associations (NFHS), and continues to lead the SMAC for the California Interscholastic Federation (CIF). Dr. Chang serves on the editorial boards of the British Journal of Sports Medicine and Sports Health, and frequently presents at national and international medical conferences. She volunteers as a team physician at UC Berkeley and Berkeley High School, continues to work with USA national team members, and is a medical consultant for the Berkeley Repertory Theatre.
|
Celina de Borja, M.D. (Pediatrics/Sports Medicine)
|
|
Dr. Celina de Borja’s areas of interest include sports and dance medicine, injury prevention, bone health, fractures and general pediatric orthopedics. She completed her pediatric residency training through Hackensack Meridian Health at Jersey Shore University Medical Center. She then pursued fellowship training in sports medicine through Harvard Medical School at Boston Children’s Hospital. During her fellowship in Boston, Dr. de Borja served as team physician for Northeastern University’s women’s field hockey and basketball teams; team physician for Newton South High School’s football team; and consulting physician for Boston Ballet School, Boston Conservatory and Berklee School of Music. Dr. de Borja has also actively served as a medical volunteer at various sports and mass participation events, including the Boston Marathon. She currently volunteers her time as a volunteer at the ODC Healthy Dancers' Clinic, which aims to improve the well-‐being and healthcare of the dance community through education, musculoskeletal screening and integration of health services. |
Rhonda Watkins, M.D., MPH (Pediatrics/Sports Medicine)
|
|
Dr. Rhonda Watkins is a former NCAA Division I champion in the long jump at UCLA and 2008 Olympian representing Trinidad and Tobago; she then completed a master’s in public health at UCLA while competing professionally in the long jump. She transitioned from athletics to medicine in 2012 when she matriculated at St Georges University School of Medicine. She completed Pediatric residency at UCSF Fresno and then completed a Primary Care Sports Medicine Fellowship at Boston Children’s Hospital where she served as fellow team physician for Northeastern University’s men’s basketball and track and field teams. Her interests include running injuries, injury prevention and return to sport after injury. |
Zachary Bailowitz M.D. (Physical Medicine & Rehabilitation/Sports Medicine)
|
|
Dr. Zachary Bailowitz attended medical school at the University of Arizona, then trained in Physical Medicine and Rehabilitation at the Carolinas Medical Center, followed by a fellowship in sports medicine at the New York Presbyterian/Columbia University. Dr. Bailowitz works in the department of orthopedics at Kaiser Oakland, where he sees a variety of patients for sports medicine and musculoskeletal conditions. Within the department, he specializes in diagnostic ultrasound, and performs advanced musculoskeletal ultrasound procedures including nerve hydrodissections, needle tenotomy, barbotage, and prolotherapy. His research interests include musculoskeletal ultrasound and regenerative medicine. |
Our Current Fellow (AY 25-26)
Alan Grusky, MD
 |
Alan Grusky MD Dr. Alan Grusky joined the UCSF Primary Care Sports Medicine Fellowship Program in July 2025 after completing a Family Medicine Residency at the University of California, Los Angeles (UCLA). Alan was born in Los Angeles, California and completed his undergraduate degree at UCLA with a degree in Psychobiology, where he also served as a Sports Medicine Intern for three years with the UCLA Men’s Basketball Team. He received his medical degree from Vanderbilt University, during which time he was the recipient of the AMSSM Galen Society Award and co-founded Project VINE, which aims to increase medical student knowledge and community engagement in nutrition and physical exercise. Throughout his training, Alan has provided medical coverage for UCLA Athletics, Vanderbilt Athletics, Nashville SC, and El Segundo High School, in addition to multiple mass participation sporting events including the LA Marathon, Rose Bowl Half-Marathon, and Life Rolls On Adaptive Surfing. His clinical and research interests include orthobiologics, diagnostic and procedural ultrasound, and lifestyle/preventative medicine. Outside of medicine, he enjoys watching and playing sports (such as basketball, tennis, golf, and spikeball), lifting weights, attending live music events, and exploring new restaurants with his wife and friends. |
Meet Our Alumni
| Year | Name |
| 2025 |
Haley Oosterhouse MD Medical School: Keck School of Medicine, USC Residency: Long Beach Memorial Family Medicine Residency Program Current Employment: UCSF Health |
| 2024 |
Frances Tao MD MPH Medical School: UC Riverside Masters in Public Health: Harvard T.H. Chan School of Public Health Residency: UCLA Family Medicine Residency Current Employment: UCLA Health |
| 2023 |
Ryan Wei MD Medical School: Temple University Residency: Kaiser Permanente Santa Rosa Family Medicine Residency Current Employment: Kaiser Permanente |
| 2022 |
Pete DeJong MD Medical School: Michigan State University College of Human Medicine Residency: Utah Healthcare Institute Current Employment: Providence Health in Portland, OR |
| 2021 |
Ginger Cupit DO Medical School: Western University of Health Sciences, College of Osteopathic Medicine of the Pacific - Northwest Residency: Georgetown University Current Employment: UCSF Health |
Thank you for your interest in our UCSF Primary Care Sports Medicine Fellowship Program. Please contact any of us or program coordinator Will Dunbar at orthoeduteam@ucsf.edu.