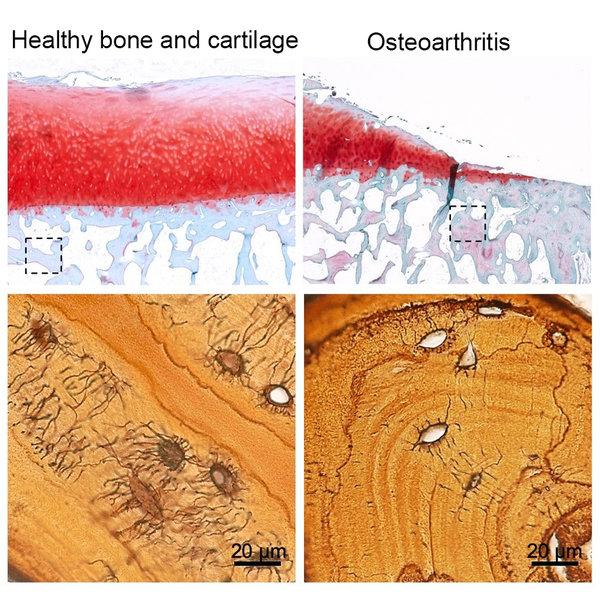
Using human tissue to study the importance of osteocytes and their relationship to bone health and arthritis, images above show the loss of connections between osteocytes in the bone that supports cartilage in arthritic knee joints. (PHOTO: UCSF Dept. of Orthopaedic Surgery)
SAN FRANCISCO (Nov. 5, 2019) -- This week, the journal Bone Research published a paper on a pivotal study of the emerging role of osteocytes and their relevance to bone health and arthritis.
 The paper, entitled "Osteocyte dysfunction promotes osteoarthritis through MMP13-dependent suppression of subchondral bone homeostasis," was first-authored by Courtney Mazur, a sixth year graduate student in the UCSF Laboratory of Skeletal Mechanobiology in the Department of Orthopaedic Surgery. Tamara Alliston, PhD, serves as the paper's corresponding author.
The paper, entitled "Osteocyte dysfunction promotes osteoarthritis through MMP13-dependent suppression of subchondral bone homeostasis," was first-authored by Courtney Mazur, a sixth year graduate student in the UCSF Laboratory of Skeletal Mechanobiology in the Department of Orthopaedic Surgery. Tamara Alliston, PhD, serves as the paper's corresponding author.
Osteocytes -- mature bone cells that become trapped within the very bone matrix they produce -- continue to remodel bone to from the inside out. Though osteocytes were primarily thought to direct the remodeling activity of other bone cell types, this study and others show the importance of bone remodeling by osteocytes themselves for maintaining bone strength and health.
In this new study, research implicates for the first time a new cell type in arthritis: osteocytes.
"Osteocytes are cells that live inside the bone and they are connected by a very intricate network of tunnels." said Mazur. "These cells have only recently started to be understood, mostly because it is harder to study cells inside the bone than on the surface of the bones."
To conduct the team’s research, they used both human tissue donated from veterans with severe arthritis, as well as tissue from sophisticated mouse models.
"We wanted to find if these osteocytes play a causal role in arthritis," Mazur said. "We looked at the end first. In humans, we knew that bone and cartilage disease often goes together. So we looked at human tissue of knee joints that had severe arthritis and required a knee replacement," she said. "We examined the osteocytes within bone that gets removed from the tibial plateau before the joint gets replaced with the artificial knee implant."
"In sophisticated mouse models, we started at the beginning and disrupted the osteocytes," Mazur said. "We made a genetically modified mouse -- a mouse that was missing a protein in osteocytes that we now know is very essential to maintaining the health of the osteocytes. The bone got less healthy, and we also saw that the cartilage looked arthritic."
Clinical relevance
"The clinical relevance adds to the scientific impact of identifying a new role for osteocytes in arthritis. This study will guide clinicians to more fully consider bone health when they are diagnosing and treating arthritis," Alliston said. "When therapeutic drugs are being developed for osteoarthritis, the impact of those drugs on the bone and specifically osteocytes need to be studied."
"This research is a great example of the collaboration in our department between basic scientists and surgeon scientists," said Thomas P. Vail MD, Chair of the Department. "These findings are a result of stellar collaboration among graduate students, post-docs, staff scientists, professors and clinicians."
Researchers were represented by: the UCSF Dept. of Orthopaedic Surgery; the UC Berkeley-UCSF Graduate Program in Bioengineering; the Department of Mechanical Engineering at the University of Utah; and the San Francisco Veterans Affairs Medical Center.
"This project was launched when it was just an idea by ‘blue sky’ funding from the Read Research Foundation,” Alliston added. "This early investment in a bold idea that could advance treatments for patients with arthritis then led to research support from the National Institutes of Health, the National Science Foundation and the U.S. Department of Defense.”
To read the full article, visit https://www.nature.com/articles/s41413-019-0070-y
###